same day & urgent walk-in appointments are available
(02) 9651 2077
3-4/286 New Line Road, Dural NSW 2158
OPENING HOURS
Monday
Tuesday
Wednesday
Thursday
Friday
Saturday
Sunday and Public Holidays
After Hours Phone Contact
8:00am - 6:00pm
8:00am - 6:00pm
8:00am - 6:00pm
8:00am - 6:00pm
8:00am - 6:00pm
8:30am - 12:00pm
Closed
137 425
CERVICAL CANCER SCREENING – WHAT’S CHANGED?
Cervical cancer is an important cancer to be aware of, and screen for, in Australian women.

CERVICAL CANCER SCREENING – WHAT’S CHANGED IN 2023?
Cervical cancer is an important cancer to be aware of, and screen for, in Australian women.
The last few years have been confusing for many women – not knowing the newest changes to cervical cancer screening in Australia and understanding how these changes impact us.
So what important information do I need to know?
What is the Cervical Screening Test (CST) – Is it different from a pap smear?
The Cervical Cancer Screening Test is a simple test to look for signs of the human papillomavirus (HPV) – a common infection that causes most cervical cancers. Most cases of HPV clear up on their own, however, sometimes it can develop into cancer. Doing the Cervical Screening Test every 5 years means your healthcare provider can monitor or investigate HPV further if needed.
The cervical screening test is slightly different to a regular pap smear in what we test for. Previously, the pap smear was done to look for abnormal cells in the cervix. The new cervical screening test (CST) is the addition of testing for HPV and is more sensitive (accurate) in picking this up. If there is any HPV strain detected on the CST, then the same sample is used to look for any abnormal cells.
The method of collecting the cervical screening test is mostly similar to the previous pap smear but there is now a self-collection option available for women to look for HPV, in addition to the doctor-collection option.
At What Age or When do I Start Having the Cervical Screening Test?
You are eligible for a subsidised Cervical Screening Test if you are:
• aged between 25 and 74
• sexually active or ever have been
• a woman or person with a cervix.
It makes no difference if you:
• have had the HPV vaccination or not
• are gay, lesbian, bisexual, transgender or straight
• are no longer sexually active
• have been through menopause
• have been with only one sexual partner
• have had a baby or are pregnant (ensure to let your health care professional know).
If you have had a full or partial hysterectomy, please check with your doctor about screening.
You are eligible to have your first test when you turn 25 or 2 years after your last Pap test. Cervical screening occurs every 5 years after that.
Why Does Screening for Cervical Cancer Only Start at the Age of 25? It used to be from 18 years old onwards, right?
This is because there are common cervical infections or abnormalities usually go away by themselves before you’re 25. Cervical cancer is also rare in this age group.
Starting to screen for cervical cancer at age 25 means we prevent a lot of unnecessary tests and treatment. The test is also more sensitive in picking up HPV and hence, the interval of 5 years between tests is because cervical cancer is a slow-growing condition and most young women will clear the HPV virus naturally.
How is a Cervical Cancer Screening Test Done?
If you choose to have your healthcare provider collect your sample
Usually, you need to take off your clothes below the waist. You lie on your back, with your knees apart. You will be given a sheet to cover yourself. You can ask for a sheet if you’re not given one.
The doctor or nurse will gently insert a speculum (a duck-bill-shaped plastic device) into your vagina, to hold it open. They will then take a small sample from your cervix using a swab. It may feel strange but should not hurt.
You may have some spotting or light bleeding which should not last for more than 24 hours after this collection is done. Please contact your GP if it persists.
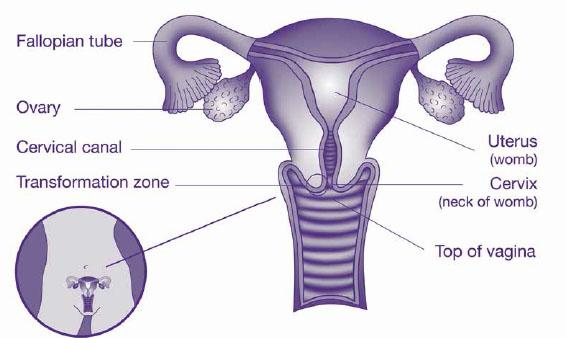
Uterus
If you choose to collect your own sample (self-collection)
Please feel free to ask your GP about this newer option. Self-collection involves inserting a swab into your vagina and rotating it for 10 to 30 seconds. This should not hurt but may feel a bit uncomfortable.
Is There Anything Important that I Need to be Aware of with the Cervical Cancer Self-Collection Method?
Because the cervical screening self-collection test looks for HPV only – not cervical cell abnormalities – it is generally not appropriate for people who have had a previous abnormal CST result or are experiencing unusual bleeding, pain or discharge.
If a self-collected sample returns a positive HPV result, you will need to return to your GP for a clinician-collected sample to assess further for any abnormal cells.
What Happens to my results?
Results usually take around 7-10 days after collection of the sample. It is recommended that you discuss all results with your GP.
• Unsatisfactory result: Indicates that the lab was unable to view enough cells in the sample and requires a recollection in 6-12 weeks.
• Normal results: usually require no follow up and followed up with another CST in 5 years
• Abnormal results: require a review with your GP and according to the result, may need more frequent CST or a referral to a gynaecologist.
Please note that a review with your GP is highly recommended if you have any bleeding outside the expected times of your cycle, including immediately after intercourse. A CST may be needed earlier than the regular screening schedule if this occurs.
How Will I Know When I am Next Due for a Cervical Screening Test?
All results get sent and monitored by the National Cancer Screening Register. If your address details are correct, you will receive a letter from them reminding you of your next CST about a month before it is due.
In addition, most GPs have reminder systems in place to ensure that patients get an SMS reminder when it is due.
If you have any further questions about Cervical Cancer Screening, please don’t hesitate to book in to see your GP today! Appointments can be made at www.dfmp.com.au or call us on 9651 2077.

This article was written by Dr Kalpana Loganath (MbChB, DCH, CWH, Clin Dip Pall Med, FRACGP), General Practitioner at Dural Family Medical Practice.
Dr Kalpana graduated with a Medicine degree from University of Auckland in 2010. She completed her internship and resident years in Adelaide before embarking on general practice speciality training.
Kalpana is also qualified with a Certificate in Women’s Health, Diploma in Children’s Health and a Diploma in Palliative Medicine which has contributed to her being able to practise holistic medicine for her patients. In addition to chronic disease management, she has special interests in women’s health, paediatrics, skin cancer management, palliative medicine and also preventative medicine.
Dr Kalpana currently bulk bills all Pension and Health Care Card Holders, as well as all children under the age of 12. To make an appointment, please visit www.dfmp.com.au or call us on 9651 2077.